Infectious Diseases
See also: Public Health; Malaria; Influenza Outbreak of 1918-1919
Part i: Overview; Part ii: Significant Infectious Diseases in North Carolina History
Part II: Significant Infectious Diseases in North Carolina History
The following infectious diseases caused serious damage to the lives and health of North Carolinians before the discovery of successful inoculations and vaccines.
Ague. An acute form of fever that often damages nerves and is sometimes fatal, ague was present in North Carolina from colonial times until the 1930s. The term was prevalent among early colonists, although ague and malaria shared many symptoms and were often mistaken for one another. In fact, little information exists that relates specifically to ague because the histories of the diseases are so intertwined.
Early colonists coined the term "seasoning" to refer to cases of ague and similar diseases. Ague and malaria began to reach epidemic proportions among white colonists after the arrival of ships carrying infected, enslaved people from Africa between 1682 and 1685. An abundance of marshland and an inadequate water supply exacerbated the problem as mosquitoes, the diseases' primary carrier, thrived in the region.
In the twentieth century, records of ague cases became more accurate. The disease was prevalent on the coast and in the Piedmont, whereas infections were rare in the Mountains. By the 1930s, enhancements in sanitary conditions and better medical treatment began to greatly lessen the threat of ague and similar diseases among North Carolinians.
Diphtheria. One of the dreaded diseases of both children and adults, diphtheria was present in nineteenth-century North Carolina. The disease is of bacterial origin, the toxin from which causes damage to the throat area with possible obstruction to the breathing passages and subsequent suffocation. Many cases described as croup before the germ theory of contagion were no doubt actually diphtheria, since it is one of the several infections that presents with a "croupy" cough.
In 1887 diphtheria was listed in official records as the third most important cause of death in North Carolina. During 1920-24 there were 25,460 reported cases, with 1,864 deaths attributed to this disease. It was not until the early 1920s that an effective vaccine for diphtheria was developed and not until 1939 that compulsory immunization for schoolchildren with the diphtheria vaccine was mandated by the General Assembly. By the early 2000s diphtheria was rare, not only in North Carolina but nationwide, and antibiotics were available for those cases that did occur.
Influenza. An infectious disease of viral origin that is worldwide in distribution, influenza, or "the flu," was first described by Hippocrates, the "Father of Medicine," in 412 B.C. About 29 pandemics were recorded between 1510 and 1918. In the great "Spanish" flu pandemic of 1918-19, after World War I, North Carolina lost 13,644 citizens, including Edward Kidder Graham, the new president of the University of North Carolina.
The causative virus of influenza was first isolated in 1933, and a vaccine was developed in the 1940s. The ability of the virus to shift susceptibility to the vaccine requires an annual change in its composition to ensure the inclusion of protection against the strains most likely to be encountered in that particular year.
Malaria. A major public health problem for decades, malaria was especially prevalent in coastal North Carolina during the early years of settlement. The disease is caused by a protozoan parasite named plasmodium. There are several varieties, all of which are transmitted from person to person by the bite of a female Anopheles mosquito. The year 1889 was a particularly bad one for malaria in North Carolina, probably due to an unusually mild winter with no killing frosts. Control of the disease was slow until 1898, when the mechanism of mosquito transmission was identified. Following this discovery, efforts at mosquito control began to see results.
In 1936 malaria was declared a reportable disease to the State Board of Health; a widespread attempt to obtain blood smears from persons in high-incidence areas was undertaken, and a concerted effort to drain swamps in these areas was intensified. Quinine became available for the treatment of malaria around 1820, although the use of powdered cinchona bark, from which quinine was derived, had been used by the Spanish in Peru as early as 1638 and to some extent in the United States. Since 1946, however, chloroquine has been the drug of choice, supplemented by quinine and related substances in resistant cases. Since 1970 North Carolina has reported only sporadic incidents of malaria, generally contracted by persons during travel to endemic areas in other parts of the world.
Poliomyelitis. A contagious viral infection, polio is manifested by an aseptic meningitis, often with paralytic results that may be permanent or, in the worst cases, fatal. The disease affects both children and adults, but because of its frequent occurrence in small children, it came to be known as "infantile paralysis." Perhaps its most famous victim was President Franklin D. Roosevelt.
Polio epidemics, occurring especially in the summer, struck terror into the hearts of American parents during the first half of the twentieth century. In 1948, an especially bad year for North Carolina, 2,516 cases and 143 deaths were reported. A special emergency polio hospital was set up in the Greensboro area since Guilford was the hardest hit county in the state. The National Foundation for Infantile Paralysis, whose annual fund-raising effort is called the "March of Dimes," was founded on 3 Jan. 1938 to help finance a nationwide campaign of education, research, and relief for victims of epidemics. In 1948 alone, the foundation  allotted more than $1.4 million to North Carolina to mitigate the statewide tragedy.
allotted more than $1.4 million to North Carolina to mitigate the statewide tragedy.
In the prevaccine era, the so-called iron lung machine-a respirator device into which persons unable to breathe for themselves because of the effects of polio were placed and artificially ventilated-became a familiar sight in all hospitals treating polio patients. In 1955 a vaccine named after its developer, Jonas Salk, became available for injection. It was quickly put into general use across North Carolina, resulting in an almost immediate decline both in new cases and deaths from the disease. In 1959 North Carolina was the first state to add the polio vaccine to the list of immunizations mandatory for children. In 1962 the Sabin vaccine, an improved preparation that could be administered orally, was introduced and soon largely replaced the injectable vaccine. The virtual abolishment of this dreaded disease in households across the nation was one of the most dramatic medical success stories of the twentieth century.
Scarlet Fever. Also known as scarlatina, scarlet fever is a febrile illness accompanied by a characteristic red rash and sore throat caused by infection with a toxin-producing strain of Streptococcus bacteria. Before the discovery of penicillin, scarlet fever could only be treated symptomatically and allowed to run its course. To prevent its spread through household contact, strict quarantine was mandated by public health officials. Epidemics of scarlet fever were commonplace in North Carolina until the advent in the 1940s of penicillin, which has been the drug of choice in treatment of this infection.
Smallpox. Also known as variola, smallpox, one of the ancient viral illnesses of epidemic and endemic proportions, was introduced into the North American mainland by the earliest European settlers. By 1711 smallpox had become endemic among the North Carolina population, including the Indians of the region. Primitive efforts of quarantine and isolation were ineffective in preventing its spread, such as the virulent smallpox epidemic in Charlotte in 1770. In 1798 Edward Jenner, an English physician, discovered that an inoculum derived from the cowpox virus, a similar but less potent pathogen, could prevent smallpox in humans. Yet many years elapsed before this type of vaccination became generally acceptable to the public, and many more years passed before it became mandatory.
In 1836 Ashe County alone reported 70 cases of smallpox. Other North Carolina epidemics occurred in Charlotte in 1851, in Salisbury in 1863, and in Wilmington in 1865. Compulsory smallpox vaccination in schools was required in Hyde County and a portion of Washington County in 1905. The State Board of Health, created by the General Assembly in 1877, led a decades-long battle to promote vaccination against smallpox. In 1911, 113 years after Jenner's development of the vaccine, the legislature enacted a statute requiring inoculation against smallpox, and in 1918 the State Board of Health made smallpox a reportable disease. Following these important public health measures, the annual cases dropped to 3,845 by 1924 and continued to decline rapidly. The last death from smallpox reported in North Carolina occurred in 1943, and the last reported case in the state was in 1953. Due to the worldwide promotion of immunization by the World Health Organization, smallpox was eliminated as a health hazard, and consequently the requirement for smallpox vaccination in North Carolina was lifted in 1973.
Tuberculosis. Sometimes referred to as the "Great White Plague" and frequently called "consumption," tuberculosis was also introduced into North Carolina by the earliest English settlers. John Lawson, in A New Voyage to Carolina (1709), noted the apparent absence of the disease among the local Indians. By the latter half of the nineteenth century, tuberculosis was the leading cause of death in the United States. Prior to the advent of antituberculosis drugs, the preferred treatment was institutional care in facilities located in a mountainous environment with pure, cool, and dry air. In North Carolina, Asheville became famous for its large number of private sanatoriums and consequently for the many physicians who specialized in the care of tuberculosis patients drawn to the area.
Tuberculosis was made a reportable disease by the State Board of Health in 1913. The first state-supported sanatorium opened near Aberdeen in April 1908; state-supported tuberculosis hospitals were later established at Wilson, Swannanoa, and Chapel Hill to permit full coverage across North Carolina.
In 1947, 1,056 people died from tuberculosis statewide. There was no effective medicine to treat the disease until the mid-1940s, when streptomycin was discovered and began to be used. Subsequently, a number of other antituberculosis drugs were introduced and usually used in combination for optimum treatment. Following the introduction of these drugs, the number of new cases began to decline. By 1962 all county sanatoriums had been closed and the residual patients transferred to one of the state-supported institutions.
In the early 2000s tuberculosis continued to be a public health problem in North Carolina. The incidence of tuberculosis was again on the increase, especially among AIDS victims. Periodic skin testing as a means of tuberculosis case-finding remained part of careful medical practice.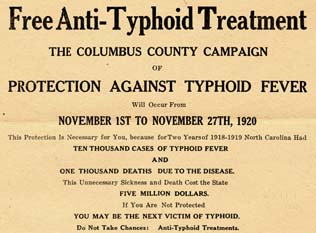
Typhoid Fever. A bacterial infection depending in large part on contaminated water and food supplies for its transmission, typhoid fever was present in endemic proportions among the earliest settlers in North Carolina. Although the first description of epidemic typhoid fever was penned by Thomas Willis in 1659, it was not until 1880 that the typhoid bacillus-the causative agent of the disease-was discovered. The first inoculations with a killed bacterial suspension began in 1896, and the vaccine had a good measure of success during the World War I years of 1914-18. After that, summertime clinics providing "typhoid shots" were commonplace across the state.
A much more effective method of controlling this disease was the effort by public health departments to clean up water, milk, and food supplies. In the 1880s municipal waterworks began to replace wells and public pumps in Raleigh, Charlotte, Wilmington, and Winston-Salem. By 1894 Charlotte, New Bern, Asheville, Winston-Salem, and Raleigh had sewerage systems. After another half century, the outdoor privy had virtually disappeared.
In 1901 there were still 8,000 to 10,000 cases of typhoid fever in North Carolina annually. In 1918, when large-scale typhoid immunization programs went into effect, the number dropped to 3,461 cases and subsequently declined steadily; after 1953 fewer than 10 cases were reported annually. The first useful antibiotic for typhoid fever, chloramphenicol, was developed in 1948; this drug and new antibiotics were very helpful in controlling the disease.
Typhus. An infection caused by a Rickettsial organism transmitted by the bites of lice that have also infested rats, typhus was endemic among early North Carolina colonists, especially in port cities where ships containing many rats in the holds and among the cargo were coming and going. In 1758, during the French and Indian War, a large number of refugees flocked to the Moravian settlement of Bethabara, resulting in an outbreak of typhus that took the lives of many refugees as well as Moravians. In 1940, when 65 cases of typhus were reported in the state, the disease became a concern of public health authorities. A major effort was directed toward rodent control and rat-proofing of buildings; by 1952, only 12 cases were reported, and none occurred by 1970.
Yaws. Still a major health hazard in many Third World countries, yaws was a crippling disease for many North Carolinians in the late seventeenth and early eighteenth centuries. Yaws is contracted through infection by a spirochete, treponema pallidum, associated with primitive living conditions. It is transmitted by skin contact and manifests itself as pimples that, on sloughing off, leave mulberrylike growths of fungi. These tend to develop into malignant ulcers that may cover the body, attacking especially glands of the armpits, groin, throat, palate, and soles of the feet. Believed to have been imported into the American colonies on slave ships from Africa and the West Indies, yaws caused many North Carolina victims to lose their noses and palates.
Physicians treated yaws by the same methods used against venereal syphilis, the symptoms of which were nearly identical. Mercury, a mixture of several kinds of barks and roots (called "papaw's remedy"), "sweating boxes" to dry up ulcers, "yaws houses" to segregate infected, enslaved people, restricted diets, and other remedies had little effect. The disease appears to have largely disappeared by 1750, although a prominent physician claimed to have found it in coastal areas of the state at the beginning of the twentieth century.
Yellow Fever. An acute viral illness characterized by high fever, jaundice, and brain disease, yellow fever is transmitted from person to person by the bite of an Aedes mosquito, which serves as the insect vector for the disease. In colonial North Carolina, yellow fever was frequently encountered in coastal settlements, especially where mosquitoes were found in abundance. For 200 years it was one of the great plagues not only of the United States but also of the entire world.
In September 1862, in the midst of the Civil War, a severe epidemic of yellow fever struck Wilmington after a blockade-running vessel from Nassau in the Bahamas loaded with supplies made its way into the Cape Fear River and docked in the port. In the zeal to off-load much-needed food and other cargo, the quarantine laws were apparently overlooked. A few days later, several Wilmington physicians reported cases suggestive of yellow fever, and it was found that there had been cases aboard the vessel from Nassau. The disease spread rapidly. Deaths numbered as high as 18 in a single day, and at one time as many as 500 cases were being treated. Physicians and nurses from as far away as Charleston, S.C., responded to the call for assistance. The epidemic lasted until 6 Nov. 1862, when a heavy snowstorm occurred. About 1,000 people died. One of the victims was James H. Dickson, a former president of the North Carolina Medical Society. The death of one of their colleagues increased the realization among North Carolina physicians that more had to be done to prevent yellow fever and other deadly contagious diseases in the state.
Progress in controlling yellow fever was slow until 1898, when it was discovered that the mosquito was the carrier for its transmission. Thereafter, widespread efforts to drain swamps and eradicate the mosquito population helped prevent infection.
There was no satisfactory vaccine against yellow fever prior to 1937. That year a substance utilizing a strain of yellow fever virus called "17D," obtained by prolonged propagation in chick embryo tissue, was found to be effective and safe for humans and used experimentally. The vaccine was available during World War II to protect troops entering areas endemic to yellow fever.
No cases of yellow fever appeared in North Carolina after the advent of modern-day reporting in 1932. In the early 2000s this disease was endemic only in South America and Africa.
Return to > Part I: Overview ![]()
References:
Thomas J. Farnham and Francis P. King, "'The March of the Destroyer': The New Bern Yellow Fever Epidemic of 1864," NCHR 73 (October 1996).
Frederick L. Hoffman, Malaria in Virginia, North Carolina, and South Carolina (1933).
Dorothy Long, ed., Medicine in North Carolina: Essays in the History of Medical Science and Medical Service, 1524-1960 (1972).
Thomas C. Parramore, "The 'Country Distemper' in Colonial North Carolina," NCHR 48 (Winter 1971).
William S. Powell, North Carolina through Four Centuries (1989).
Benjamin Earle Washburn, A History of the North Carolina State Board of Health, 1877-1925 (1966).
Jane Zimmerman, "The Formative Years of the North Carolina Board of Health, 1877-1893," NCHR 21 (January 1944).
Additional Resources:
Watson, Alan D. “Combating Contagion: Smallpox and the Protection of Public Health in North Carolina, 1750 to 1825.” The North Carolina Historical Review 90, no. 1 (2013): 26–48. http://www.jstor.org/stable/23523656.
Image Credit:
Pamphlet from Polk Diphtheria Cure Co. of Boston, Massachusetts. Image courtesy of the UNC-CH libraries. Available from http://www.lib.unc.edu/blogs/ncm/index.php/2009/05/29/a-cure-for-diphtheria/ (accessed August 20, 2012).
"Iron lung (c. 1933) used to "breathe" for polio patients until 1955." Image courtesy of Library of Congress. Available from http://www.loc.gov/pictures/resource/highsm.05216/ (accessed August 20, 2012).
Free Anti-Typhoid Treatment. The Columbus County Campaign of Protection Against Typhoid Fever Will Occur from November 1st to November 27th, 1920. Image courtesy of University of North Carolina at Chapel Hill Libraries. Available from https://docsouth.unc.edu/nc/antityph/menu.html (accessed August 20, 2012)
1 January 2006 | Cockrell, David L.; Hosfeld, Andrew; Norris, David A.; Parramore, Thomas C.